- Home
- SLIPPED DISC
- Lumbar disc protrusion
- Home
- SLIPPED DISC
- Lumbar disc protrusion
Lumbar disc protrusion
Lumbar disc protrusion says take LBP seriously and you probably will not end up under the knife.
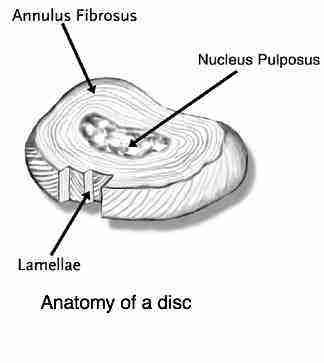
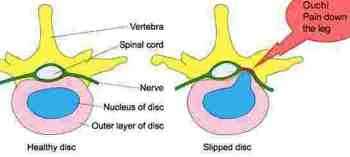
The terms prolapse, herniation and slipped disc are used very loosely and probably confusingly for you. All of them involve a degree of damage to the annulus fibrosis and protrusion of the nucleus pulposis beyond its normal confines.
The question is has the tear gone deep enough to allow the bulge to pinch the nerve?
That could be the sciatic or femoral nerve; the former emerges from the lowermost lumbar spine and the latter somewhat higher.
Here is the trick. Take your grade one lumbar protrusion, also known as a mild slipped disc, seriously. Do what it takes and wait long enough for the annulus fibrosis to heal; that is six weeks. Even though the pain may have ceased, recognise that it takes, yes, at least one and half months to mend.
Do not move the grand piano. Do not go back to gym yet, or at least be very careful. Try not to sit more than you need to. Avoid a long journey by car. Bend very carefully, and better still go down on one knee to pick up your shoes off the floor. And lastly it makes no sense to disguise the pain with anti-inflammatory pills, analgesics or muscle relaxants.
Do the exercises faithfully. Start walking daily, and better still swimming too. Do use the ice and heat when you have the occasional less than optimal day.
Lumbar surgery is a huge cost to medical insurance and whilst it is sometimes necessary, often it comes about when a person, not you, of course, hurts their back but returns to normal activities before it has healed.
Do all this, then you, and your chiropractor will be happy. The only person who might be unhappy is the neuro or orthopaedic surgeon. They have just lost out on their annual skiing holiday in the Swiss Alps that you were about to sponsor.
Lumbar disc protrusion
At the CHIROPRACTIC COALFACE I find it useful to think of FIVE levels of a lumbar disc protrusion or herniation. Disc and disk are used interchangeably.
More traditionally, it is considered that there are four levels of slipped disc.
Lower back and leg pain
Acute lower back and leg pain is a nightmare, especially if you have a deep ache when coughing and sneezing, or bearing down on the toilet; even laughing. Then it is best to assume you have a lumbar disc protrusion; but how bad is it?
- Grade I: A bulge of the disc causing lower back pain with no leg pain
- Grade II: A bulge of the disk causing low back pain and the first symptoms in the leg: tingling, pain, a numb feeling, but on testing there is no difference between the legs.
- Grade III: Low back pain but now there is measurable difference on testing between the sensation in the legs. Prick the naughty leg and it's quite different to its compatriot in certain parts of the leg, more about that later. Now we are talking about the first signs of prolapse.
- Grade IV:
Lower back pain, but now there is a feeling that the leg is becoming
weak. You have difficulty standing on your toes, or you can't lift your
big toe, which might make you trip, or your knee gives on the stairs. A
progressing prolapse. Herniated disc foot drop.
- Grade V: This is the true, fully developed herniated disc. Often the lower back pain is less intense, but the leg is on fire.
- Chiropractic Conditions is a central page at our site. It provides you simply and easily with the sorts of diagnoses that the average DC would be treating.
- Healthy Living Tips is another vital page at Chiropractic Help. Sparkling wellbeing is not just about having your subluxations adjusted. This link gives you some insights into different foods you could and perhaps should be eating.
Obviously I am speaking in jest. No doctor, especially highly qualified surgical specialists are worrying about where their next holiday is coming from. Nor do they want your grade one slipped disc to turn into a level five surgical emergency.
Look after the pennies and the pounds look after themselves. Care properly for a small lumbar disc protrusion and you will not have to be concerned about a grade five and lower back surgery. Because, when the back pain stops, and the leg is on fire, the chances that conservative treatment like chiropractic can help you become much less.
This lumbar disc protrusion casefile will make interesting reading.
Mr S, a 38 year old man consulted me three weeks ago with severe left low back pain, with no radiation to the leg; thus a grade one.
Nine months ago he had a knee operation that went sour; in hospital he got a serious infection in the knee during the operation, and for five months he had difficulty walking and developed a marked limp.
Gradually, with the help of powerful antibiotics he got over the infection that he acquired in hospital and was able to start exercising again. In the interim he had put on quite a lot of weight. He started to jog gently and even playing tennis.
Then, two weeks ago, after a game of tennis he developed nagging lower back pain, but it passed over within 24 hours with the help of anti inflammatory pills.
Then, the evening before his first consultation, now three weeks ago, he again played tennis. That night he developed severe lower back pain. He couldn't sleep, and every move in bed caused sharp pain in the back. In the morning he felt completely disabled and his back felt like jelly. His wife had to put his shoes and socks on; every movement causing sharp stabs of pain in the lower back. A sneeze gave him a very disabling sharp stabs of pain.
He reported that as a teenager he had two compression fractures in the lower back from a heavy rugby tackle.
- What is IATROGENIC ILLNESS? It's the third most common disease on the planet.
Help for sciatica pain
A lumbar disc protrusion doesn't normally affect the nerve directly though it is threatened; but the treatment is much the same as help for sciatica pain.
Mr S stood in a "stuck forward" posture, known as "an antalgia", a posture that the lower back adopts to protect it from further injury. Usually an antalgia is a sign of herniated lumbar discs but a facet syndrome can also cause it, mainly in the older person.
The Valsalva test was positive, strongly suggestive of a lumbar disc protrusion. Bearing down gave him sharp low back pain.
Forward flexion was very guarded, invoking the "jello-like" feeling in his back. As though it was suddenly going to collapse. Lumbar extension, and side bending bilaterally were also very painful.
The Slump test for sciatica was extremely painful when raising the left leg, and slightly painful when raising the right leg, but only in the back. The Straight Leg raise test of Lasegue was extremely painful at 15 degrees on the left, again fortunately only lower back pain.
There was a L4 lumbar spine fixation on motion palpation.
There were no abnormal neurological findings.
Two dilemmas
The clearcut diagnosis was a small lumbar disc protrusion, Grade I, with no involvement of the sciatic nerve at that stage.
To X-ray, or not to X-ray, that was the question. The reasons in favour of an X-ray were the old compression fractures and the very severe pain. The reasons against were:
- Getting to the X-ray department over the weekend would be a nightmare, and would probably aggravate the condition.
- There would be a delay of several hours in reducing the herniated lumbar disc.
- The radiation exposure, not to be underestimated. According to a research paper published in the Lancet, a prostigious British medical journal, roughly 700 of the new cancer cases diagnosed each year in the UK are caused by medical X-rays. Did the benefits outweigh the risks? I decided not, but told him that if pain began in the leg, or he wasn't much improved with three days, then an X-ray would be mandatory.
- The cost of an X-ray. They're not cheap.
The second dilemma was a holiday booked that would involve eight hours in the car. I told him and his wife that it was highly likely they would have to call off their holiday.
HOME INSTRUCTIONS for a Lumbar Disc protrusion
- Mr S was not to sit at all for three days.
- He should ice his back at least twice a day. Cold hot therapy ...
- Forward bending was strictly verboten. He should go down on one knee if he needed to pick something off the floor.
- He should immediately blow his nose if he felt a sneeze coming on.
- He should do our three basic lower back exercises for a lumbar disc protrusion every 15-30 minutes. They take only forty seconds.
- He should spend three days on his bed*, doing the exercises, and at least every hour get up and walk around.
- Pain is your friend. I recommended he take no pain killers.
- He must listen to his back; it would tell him further what he could and couldn't do.
* Bed rest is controversial. There is much research confirming that bed rest alone
aggravates a lumbar disc protrusion. However, if the patient is not to
sit, and can't stand for any length of time... he's between the devil
and the deep blue sea; my slipped disc rules.
My compromise is three days' bed rest with regular exercises and getting up hourly to walk about.
PROGRESS
First treatment (Sunday): I made sure he could do the basic three exercises correctly. Whilst he could get them off the website, there's no substitute for a experienced professional showing the patient EXACTLY how they should be done. Acute pain is frightening, and many patients are anxious about the exercises. The movement helps to bring nutrients to the damaged tissue, fresh oxygen, and removal of the waste inflammatory products that would be building up.
Soft tissue massage whilst lying on his side. Lying prone on the belly often increases acute low back pain.
A gentle side-posture manipulation, with the painful side down, using a standard spinous-push manoeuvre. We both felt and heard the offending bulging nucleus pulposis reduce back to its correct place. The adjustment (manipulation) was not painful.
Second treatment on Monday: Mr S was substantially better. He stood upright and the slump test was negative. Surprisingly, there was a right sacroiliac fixation. I used the standard Thompson drop protocol, with no side posture manipulation. I carefully outlined the 50 percent less pain rule to him, warning him that a set back would almost certainly mean radiating pain down the leg.
Third treatment on Tuesday; Mr S had almost no pain. He's taken everything very seriously; he wants to go on holiday despite a potentially devastasting lumbar disc protrusion. His mother has had a two back operations so he knows what it's about.
I repeated the side posture manipulation,
again lying only on the painful side down. We both felt a much smaller
click, probably from the facet joint. I then did a supine AP drop
technique on the fixated right sacroiliac joint.
I allowed him to go on holiday provided he make room in his suitcase for
the icepack; probably not necessary, but just in case, and the
exercises, and provided he could lie down in the back of their SUV
whilst she who must be obeyed drove. Have you got one of them at home?
I gave him a more difficult exercise to strengthen the core muscles, to be done cautiously if his back would allow it.
Fourth treatment (10 days later): Mr S had no pain. He reported that after the long drive his back was a little tender, no real pain, and for two to three days he was very careful on the beach, doing backstroke regularly in the pool. Then everything stabilised. He drove most of the way home with minimal discomfort.
Range of motion was full and free, there was still a mild fixation of L4 lumbar spine. We repeated the gentle side-posture manoeuvre. I gave him a new, more difficult exercise, and asked him to return in three weeks.
DISCUSSION
Was this a misdiagnosis?
Critics would say that there is absolutely no possibility that a lumbar disc protrusion could have responded so quickly.
My reply is that the pathognomonic signs of a lumbar disc protrusion were clearcut: pain on forward bending, the antalgic posture, the extreme disability and "jelly-like" feeling, pain with a Valsalva and a very strongly positive Lasegue and Slump tests.
Prompt reduction of the protrusion
Our chiropractic experience is that if herniated lumbar discs are reduced with twenty-four hours, before swelling and inflammatory products are produced (and preferably within twelve hours) an uncomplicated lumbar disc protrusion will often respond very quickly to chiropractic care.
If that critical first 24 hour period is missed and he waited three days, there was a strong possibility that leg pain would have started. Wait three months, messing about with pills... and he has backache for life.
Following instructions...
Mr
S was a model patient. He followed my instructions to the letter, and
benefitted accordingly. So many people wish to continue with their
normal life, especially sitting, not stopping smoking, and bear the
consequences. Uncomplicated lumbar disc protrusions, neglected, often
proceeds to the full blown herniated lumbar discs, aka a lumbar disc
prolapse.
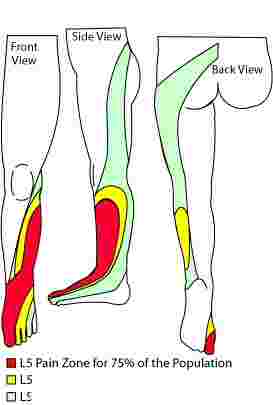
The L4-L5 disc would classically produce pain and tingling down the side of the leg and stretching over to the great toe. The medial hamstring reflex would likely diminish, there would initially be hypER sensitivity (increased) in the web between the great and second toes, later hypO (numbness) and he might develop difficulty lifting his great toe.

The "crossed" sciatic sign
If raising your left leg in the so-called Slump Test gives you more right lower back pain, it's both a good and bad sign.
Good? Because the crossed sign means you have postero medial slipped disk which are usually easier to manage with chiropractic adjustments if there is no significant leg pain.
Bad? Because a higher percentage of patients with the medial disc end up under the knife. Read about it at the link just above.
One particularly nasty sign: if raising the left leg as in the graphic above, gives you RIGHT leg pain, then it's going to be difficult.
Femoral nerve
The femoral nerve emerges from higher in the lumbar spine and supplies predominantly the front of the thigh and the inner lower leg; it is the motor nerve to the quadriceps muscle. Weakness causes a profound limp. Lumbar disc protrusions are equally serious.
Femoral nerve lesions tend to occur more often in the older person.
Here is my own personal scrape with femoral nerve damage; ouch, it hurt.
Bernie's blog:
Beer makes a good servant but ...
ANECDOTES
Always treat anecdotes like this on the web with a certain amount of skepticism. Even by my standards, Mr S responded remarkably quickly. Anecdotes are not scientifically proven remedies.
But the underlying principles are valid: take a small problem seriously, exercise is always vital, (the right exercises), reduced sitting is usually necessary and ice makes a good anti inflammatory and painkiller.
And get the bulging disc reduced as soon as possible, no matter how much pain you are in. By an experienced chiropractor preferably, but there I am obviously biased! By some local doctor you trust.
In the minds of some this is an immediate surgical emergency; an interestingly if you FIRST consult a medical person with an acute lower back condition, the chances of you ending up under the knife are much greater; add to that the considerable dangers of a general anaesthetic, and it's worth considering conservative treatment like chiropractic.
Useful links
Useful links brings you allied pages if you are suffering from a lumbar disc protrusion.
- Valsalver manoever- pain with coughing or sneezing?
- Slipped disc rules
- Go from LUMBAR DISC PROTRUSION to LOW BACK PAIN homepage …
- Home
- SLIPPED DISC
- Lumbar disc protrusion
Did you find this page useful? Then perhaps forward it to a suffering friend. Better still, Tweet or Face Book it.

