- All You Need to Know
Lumbar Facet Arthropathy Spondylolysthesis
This is a not uncommon condition found at the chiropractic clinic. It's often associated with severe leg pain.
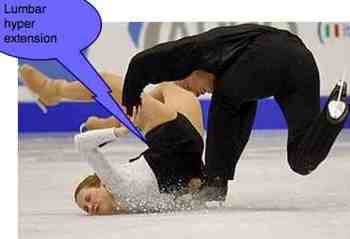
The lumbar facet joints are subject to wear and tear, particularly after a hyperextension injury that was not properly cared for. The ensuing chronic fixation leads invariably to immobilisation arthritis[1] and hyaline cartilage degeneration.
In short, the hyaline cartilage that lines the ends of bones is dependent on movement for correct nutrition. Immobilise or fixate a joint and it rapidly becomes arthritic.

Spondylo-lys-thesis
Shall we start by getting this jaw breaker out of the way, otherwise you my be tempted to leave this page immediately!
Spondylolysthesis is a spinal condition where one vertebra slides forwards on its neighbour below. There are two main causes:
1. Trauma which fractures the "pars", usually in childhood, but it's also a stress fracture the sportsmen get. It is very common in cricketers; fast bowlers get it.
2. Degenerative change (arthropathy) in the facet joints causing the shape and orientation to change, allowing the vertebra to slide forwards. It occurs in the older person.
This page was last updated by Dr Barrie Lewis on 9th January, 2023.
- LUMBAR FACET ARTHROPATHY ... what is it?
- Hyaline cartilage
Lumbar facet syndrome
Lumbar Facet Arthropathy Spondylolysthesis
CASE FILE
Mrs G is a 75-year old woman who has had pain in her left buttock for five years. Four months ago she fell down five steps on her buttocks (the staircases in the Nederlands are very steep). A month later the pain started radiating down her the back of her thigh and calf, with tingling on top of her foot.
She couldn't use any power with her left leg without severe pain in the leg. Turning her torso left and right, and straightening up after bending was very painful. The pain in her leg was constant, 24 hours per day. She could never escape it.
EXAMINATION
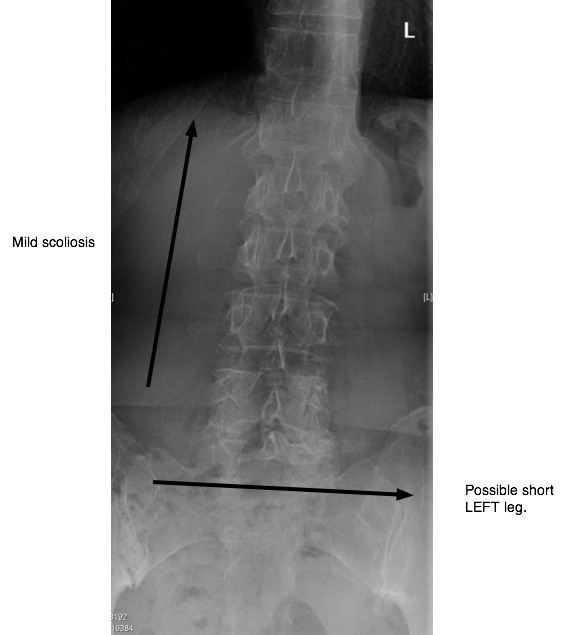
- Looking for a Leg Length Inequality is always tricky. It cannot be
measured precisely without a special X-ray of the pelvis, which I didn't
have, and sometimes it changes after adjusting the SI joint, or even the foot. However by eye-balling her pelvis, there was no
obvious low side. A mild scoliosis (curvature) however was clearly
present.
- There was a marked fixation in the opposite (right) sacroiliac
joint, and at the L5-S1. L4 was tender on
palpation.
- Forward bending caused moderate pain in her back and
buttock but did not radiate to the leg. Sideways bending, right and
left, were mildly uncomfortable.
- The test of Lasegue for a pinched nerve was very mildly positive at 60 degrees, with pain in the buttock, but not the leg. The Slump test too was mildly positive.
- SLUMP TEST for sciatica for a pinched nerve.
- There was no numbness or muscle weakness and the reflexes were normal.
- The piriformis muscle was very tender with active trigger points.
- PIRIFORMIS SYNDROME ...
- Her right hip shows signs of early arthritis. Limited flexion, adduction and internal rotation with pain in the groin.
- HIP ARTHRITIS ...
LUMBAR STENOSIS
LUMBAR FACET ARTHROPATHY SPONDYLOLYSTHESIS
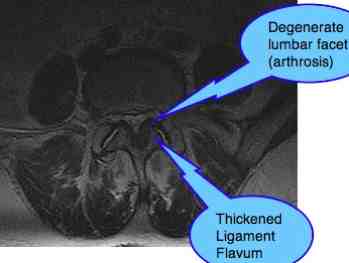
The radiological report reads:
"Forward slip of the body of L4 in relation to L5, spondylolisthesis, grade 1.
At L4-5 a canal stenosis is seen with facet arthropathy and hypertrophy (thickening) of the Ligament Flavum. Reduced intervertebral foramena right more than links.
At L5-S1 there is also relative canal stenosis, also on the basis of advanced facet arthropathy and hypertrophy of the Ligament Flavum. There is possibly a small synovial cyst at the left facet joint."

Certainly there is a very small, tight spinal canal, consistent with our case history and findings. Chronic low back and buttock pain radiating to the left foot.
Can manipulation possibly help? Does chiropractic help have a spinal stenosis explanation and solution?
DISCUSSION of LUMBAR FACET ARTHROPATHY SPONDYLOLYSTHESIS
Something didn't quite fit. With such severe pain in the leg, I would in the first place have expected pain in the limb when she bent either forwards, sideways or backwards; and that the tests for a pinched nerve would be strongly positive.
But no, this is not a pinched nerve in the normal sense, but irritated and severely inflamed by the complex toxins exuded by fixated joints.
We had to wait a week, before starting the treatment, for the x-rays
and scan which brought forth the explanation. Extremely degenerate facet
joints at L4 on 5 that had allowed the fourth lumbar vertebra to slide
forwards; spondylolysthesis.
Interestingly her symptoms were partly from the S1 nerve root from the fixated L5 joint and partly from the L5 fibre causing tingling on top of her foot from the spondylolysthesis.
The severe fixation in the right sacroiliac joint anatomy was central to the whole problem.
Treatment: lower back and leg pain
The first three treatments involved the sacroiliac joints and L5 using the Thompson drop protocol, and gentle drop treatments on L5 with her in the side-lying posture. The pain increased after the first two treatments. She was dubious, but I assured her that was normal for a chronic condition.
I modified the treatment to include the very degenerate L4-5 joint. From the case notes:
"Flex iets Li bil. Kemp R en L > Links L5. L5R vast. ZSLR L licht in L bil. L4R, L5L roll drops. Steeds pijn, dus: Prone: R sac hard, L si AS hard. Supine R en L Si, ant bekken. Active release therapie aan de linker hamstring, piriformis en Iliotibial band."
Within five treatment she had 50% less pain, and after seven it had completely gone.
We are now busy with rehab, still concentrating on the right hip arthritis which is still tender, though also improving, and I'm pondering the need for a heel lift.
Next week we start with a full examination of her neck, which is also stiff and painful.
PROGRESS
LUMBAR FACET ARTHROPATHY SPONDYLOLYSTHESIS
Mrs G came in today for her seventh treatment. She's smiling and so am I. She played tennis twice this week, with no ill effect. I am no longer so happy; that was not allowed, but it seems with no negative results.
She added a sentence about the loneliness of growing older. The tennis club is her solution. So be it, she's not just a back.
The pain in her left leg has completely stopped and the Slump test is negative. She still has a little discomfort in the right sacroiliac joint, something she has had for years, which is connected to the arthritis in her hip.
The right groin is still a little
painful when she rotates her hip. We are working on it. Rome wasn't built
in a day; nor were Aachen or Cologne as we say in Europe.
They are both worth a visit, by the way. Especially the Dom in Aachen which is where you'll see the remains of Charlemagne. The Christmas fair in Cologne is generally acknowledged as the best in Europe; and the chocolate museum is to die for.
Managing these complex cases successfully means addressing each and every part of the syndrome. A mixture of symptoms and signs, in this case the
- Muscular condition in her left buttock, the Piriformis.
- The fixation at L5.
- The spondylolysthesis at L4.
- The hip arthritis on the other side.
- Thinking about the Leg Length Inequality, and would a heel lift help, or hinder.
- Convincing the patient of the need to do daily rehab exercises, to start walking more and sitting less.
- Persuading them to accept that some things belong to the past. Can they still garden, play tennis, or work in a bookshop where lifting heavy boxes is required.
LOWER BACK AND LEG PAIN
LUMBAR FACET ARTHROPATHY SPONDYLOLYSTHESIS
Lower back and leg pain is an every-day event in chiropractic clinics. It's our bread and butter. Sometimes it is routine and straightforward, but it can be extremely complex. Occasionally we have to refer patients for surgery.
More often it's we who are trying to cope with very unhappy patients after Failed Back Surgery (FBS) as it is known in the literature, or the complications of a difficult operation.
COMPLICATIONS OF SURGERY
Today I had a new patient in her upper fifties with a not dissimilar history, but she went for the surgery. Immediately after the operation she developed a severe foot drop, and could only move about with a walker for two months.
And she still has disabling numbness and tingling in her lower leg. The X-ray reveals another LUMBAR FACET ARTHROPATHY SPONDYLOLYSTHESIS; I wonder what we can do for her, if anything.
My point is that these serious cases of degenerative lumbar spines are an every day affair in chiropractic clinics. Each has to be managed carefully, thoroughly and mostly fairly gently though periodically a good "pak sla" is necessary; a good hiding.
Do we chiropractors always win with these difficult cases? No, of course not, but isn't conservative treatment always worth a try before going for surgery?
It's never far from my mind that a favourite relative died (literally) after her seventh lumbar surgery, aged forty-two. And it all started with a routine, uncomplicated lower back strain. You can do a lot more damage with a knife in your hand, than just a plain chiropractic adjustment; plus the risk of infection, not to mention Anaesthetic Alzheimers.
Did you find this page useful? Then perhaps forward it to a suffering friend. Better still, Tweet or Face Book it.
