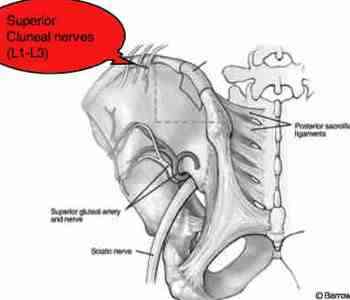
Superior cluneal nerves
Superior cluneal nerves are little known outside of the anatomical and surgical fraternity, yet they have a very important place in clinical chiropractic practice. They supply the skin of the greater part of the buttock, overlying large structures such as the gluteal muscles, the piriformis and the sciatic notch creating complex and oft confusing pain patterns.
Some anatomists believe they supply the groin too.
Orthopaedic surgeons have to be particularly careful because the nerves course over the iliac crests just where they like to harvest bone chips for a fusion.
It is easy to assume that pain in the buttock is from the gluteus maximus, or a piriformis syndrome, or a sacroiliac joint condition.
Likewise, overlying the sciatic notch, it's easy to assume this is a lower lumbar condition causing radiating pain to the buttock. And, because it often occurs simultaneously with a L5 or S1 lesion that is causing posterior thigh pain, it is missed.
As has been well said, remember the patient can have two diseases; he can also have 2 different pinched nerves causing buttock pain, one sciatic which is motor to the gluteals and the other superior cluneal supplying the overlying skin.
In its pure form, unadulterated by lower lumbar complications, the Slump test for sciatica and the straight leg raise of Lasegue will be negative.
Superior cluneal nerves
Superior cluneal nerves overlie the gluteal and piriformis muscles and the upper sciatic notch creating a confusing clinical picture.
Buttock pain can be referred from the upper lumbar spine, and have nothing to do with the sacroiliac, hip or L5 area.

Buttock pain
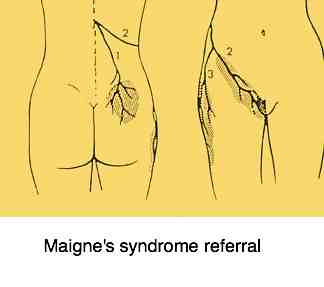
Right buttock pain is a typical feature of Maigne's syndrome and a superior cluneal nerve referral, but many other conditions too.
Right buttock showing referral pattern. Above the more traditional diagram, and below Dr Maigne's pattern.
They supply a large area of the skin of the buttock reaching from the iliac crest, down towards the posterior hip. Testing the skin for numbness, as compared to the contralateral side, using a Wartenberg pinwheel, is a key part of the examination.
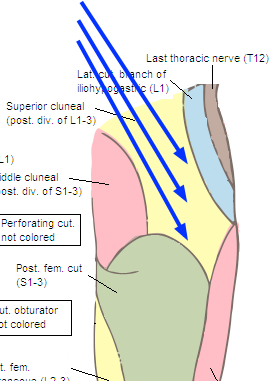
The superior cluneal nerves emerge from the mid to upper lumbar spine.
Unlike the much thicker and better known femoral nerve, however, which comes from the anterior rami of the nerve roots in the same general area, the superior cluneals find their origin in the posterior ramus of L1, L2 and L3, arrowed in red.
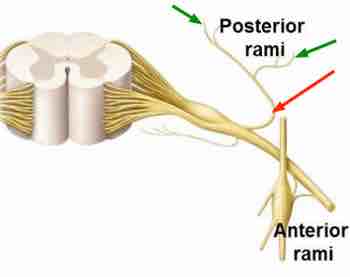
This posterior ramus splits into two branches, arrowed above in green. The medial may become involved in a so called double crush syndrome as it passes through a fibrous tunnel as it crosses the iliac crest; this may be a site of entrapment, in addition to that in the spine itself.
In short, these nerves emerge just below the thoraco lumbar junction, in itself a transitional and less stable area of the spine.
It is at this point that a lumbar scoliosis often has an apex, changing direction and providing fruitful ground for subluxations of the spine.
The area may be further complicated by small rudimentary ribs if there is an anomaly occurring at the lumbo sacral junction.
French orthopaedic surgeon Dr Robert Maigne described a syndrome, named after him, in which a facet joint subluxation in the upper lumbar spine can irritate the superior cluneal nerves with referred buttock pain. Interestingly he also claimed that irritable bowel syndrome may be similarly caused.
Chiropractors are faced on a daily basis with patients complaining of buttock pain. It takes a careful and thorough examination to determine whether the source is the sacroiliac joint, a bulging disc or a Maigne's syndrome irritating these nerves.
One can adjust the SIJ or lower back until the cows come home, but they will get minimal relief if the source of the irritation is in the upper lumbar spine.
They are purely sensory nerves with the exception of the multifidi muscles, lying between segments in the spine; they have no motor function in the buttock or leg and so will not cause distal weakness as a sciatica or femoral lesion can do.
If there is wasting of the gluteus maximus, known as the seagull sign, then one should look elsewhere for the origin of the pain and weakness.
Chiropractic adjustment of this part of the spine is particularly difficult, being a transitional area. One may use a P to A thrust with the patient lying prone, or a hyperextension technique with the fists in the small of the back.
A chiropractic lumbar roll may be more successful though L1 is often stubborn, and brute force and ignorance merely causes pain. A prone drop using the Thompson table may be more successful, or the Gonstead knee chest.
Maigne's syndrome
These Maigne's syndrome exercises will help with irritated superior cluneal nerves.
Using your hands under your back to you can do specific exercises for the T12-L1-L2-L3 area. These Maignes syndrome exercises are simple to do; every morning BEFORE getting out of bed.
Useful links
Did you find this page useful? Then perhaps forward it to a suffering friend. Better still, Tweet or Face Book it.
